Clinical Data Management (CDM) is a continuous process and a crucial component of clinical trials. CDM starts with designing the case report forms and database design in the first stage and goes on to data capture, data cleaning, data reconciliation, medical coding, and data validation in the second stage. In the third stage, clean data is locked and archived. Errors or inconsistencies in this data can have significant consequences, including patient safety risks, regulatory non-compliance, delayed approvals, and compromised trial outcomes. To mitigate these risks and ensure data of the highest quality, CDM professionals must implement robust data reconciliation and quality control practices.
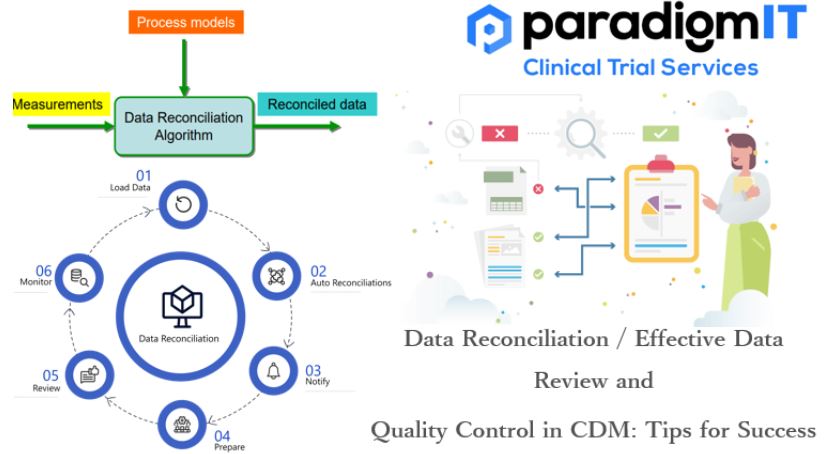
Data Reconciliation:
Data reconciliation is a process that involves comparing and aligning data from multiple sources to ensure consistency, accuracy, and integrity. The primary purpose of data reconciliation is to identify and resolve discrepancies or differences between data sets and make them consistent.
Key aspects of data reconciliation:
- Data Sources: Data reconciliation typically involves data obtained from different sources or systems. These sources can be databases, spreadsheets, sensors, or any other data collection method.
- Comparison: The data from these sources are compared to identify inconsistencies or discrepancies. These inconsistencies can be in the form of numerical variances, missing data, or conflicting information.
- Alignment: Once discrepancies are identified, the data reconciliation process works to align the data. This may involve making corrections, adjustments, or interpolations to ensure that the data from different sources match or are compatible.
- Validation: After alignment, the reconciled data is validated to ensure that it meets predefined criteria for accuracy and reliability. This often involves performing validation checks or calculations to verify the correctness of the reconciled data.
- Documentation: Throughout the process, detailed documentation is maintained to track the changes made during reconciliation. This documentation is important for audit trails, compliance, and transparency.
Importance of Data Reconciling:
Here are key reasons highlighting the importance of data reconciliation in clinical research:
- Data Accuracy and Integrity: Ensures that the data collected from various sources (e.g., electronic data capture systems, paper records, laboratory reports) are accurate and consistent. Helps identify discrepancies or inconsistencies that could compromise the reliability and integrity of the trial results.
- Patient Safety: Supports the accurate capture and reporting of safety-related data, such as adverse events and patient outcomes, ensuring timely and appropriate intervention if safety concerns arise during the trial. Contributes to monitoring and identifying any potential adverse effects of investigational drugs or medical devices, enhancing patient safety.
- Regulatory Compliance: Assures compliance with regulatory requirements and standards set by health authorities (e.g., FDA, EMA, ICH-GCP), which demand accurate, complete, and reliable clinical trial data. Facilitates adherence to regulatory guidelines for data management, which is crucial for successful trial submissions and approvals.
- Data Quality Assurance: Enhances the overall quality of clinical trial data by detecting and rectifying errors, inconsistencies, and inaccuracies, providing high-quality data for analysis and reporting. Supports a data-driven approach to decision-making by providing trustworthy, error-free data for statistical analysis and interpretation.
- Data Consistency and Uniformity: Ensures consistency and uniformity in the data across different phases of the trial, various study sites, and different data collection methods. Enables meaningful comparisons and analyses by aligning data from diverse sources, allowing for accurate trend analyses and outcome assessments.
- Reduced Risk and Improved Decision-making: Mitigates risks associated with inaccurate data, preventing potential delays in trial timelines, regulatory approvals, or market entry of investigational products. Facilitates informed decision-making throughout the trial, optimizing resource allocation and allowing for timely adjustments in trial protocols and strategies based on accurate data.
- Audit Readiness: Provides a clear audit trail of data reconciliation activities by creation of detailed records encompassing data sources, transformations, and quality control procedures. Continual maintenance ensures that record remain up-to-date which accurately reflects data modifications, resolutions, and changes in it. These facilitate compliance during regulatory audits and demonstrating transparency in data management practices.
Effective Data review and Quality control in CDM:
Following are key strategies and best practices for achieving effective data review and quality control in CDM:
- Develop a Data Review Plan
- Data Validation Checks
- Query Management
- Data Cleaning Tools
- Documentation
- Regular Data Review Meetings
- Risk-Based Quality Management
- Improvised processes/Operational Excellence
- Data Review Metrics
- Training and Mentorship
- Collaboration and Communication
Tips for Success – To preserve data quality:
- Define Data Quality Objectives: Clearly define the data quality objectives specific to your project or organization.
- Prefer the right tools: that are 21CFR Part11 compliant. Ensure that the data collected meets the regulatory requirements and has effective flags on data quality problems (e.g. EDC, IRT, ePRO/eCOA Software)
- Standardized Data Entry at Site Level: Enforce data entry standards and conventions to ensure uniformity. Use drop-down menus, predefined options, and validation lists to reduce the likelihood of data entry errors.
- Prioritize data protection: Avoid any accidental or intentional data corruption.
- Process optimization using platforms: Integrate data from different systems (which are functioning in silos).
- Proper Documentation: Verify the procedures are as per the trial protocols.
- Perform internal and participate in regulatory audits: Periodically identify non-compliance and address deficiencies in the overall CDM process.
In conclusion, data reconciliation and quality control are indispensable pillars of Clinical Data Management (CDM) that ensure the integrity and reliability of clinical trial data. By implementing the tips for success outlined in this guide, CDM professionals can uphold data quality, regulatory compliance, and patient safety, ultimately contributing to the success of clinical trials and the advancement of healthcare research.
For more information –
Visit our website – www.paradigmit.com
Or you can write us at ask@paradigmit.com Follow us for more – https://www.linkedin.com/company/paradigmittechnologyservices/?viewAsMember=true